MindMap Gallery French chemist
French chemist
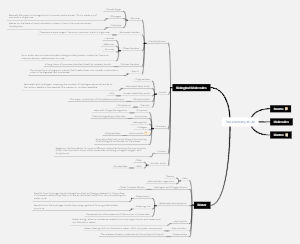
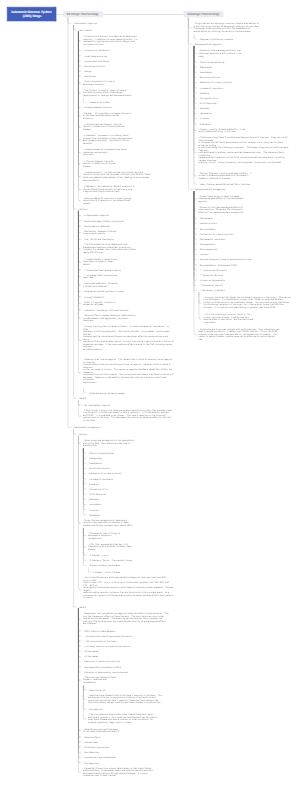
The French chemist section introduces notable French chemists and their significant contributions to the field of chemistry. Chemists such as Lavoisier and Pasteur proposed important theories such as the oxygen theory and the microbial theory of disease. These contributions have not only promoted the development of the chemical discipline but also had a profound impact on the chemical industry and social development.
Edited at 2024-12-04 13:26:05French chemist
- Recommended to you
- Outline