MindMap Gallery Principle of buffer solution
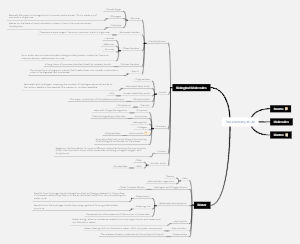
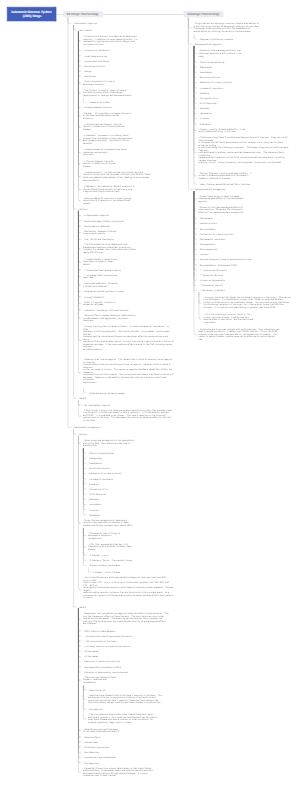
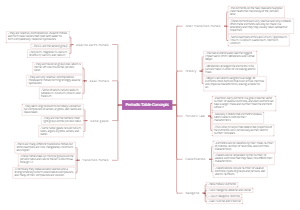
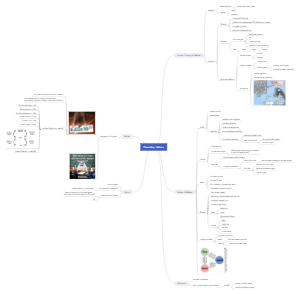
Principle of buffer solution
The principle of buffer solutions involves the components, buffering action, and preparation of buffer solutions. Buffer solutions are composed of a weak acid and its conjugate base (or a weak base and its conjugate acid), which resist changes in pH. The buffering action is achieved by accepting or releasing hydrogen ions, thereby maintaining the stability of the solution's pH. To prepare a buffer solution, one needs to choose the appropriate buffer pair and calculate the required concentrations to ensure its buffering capacity.
Edited at 2024-12-17 02:54:09Principle of buffer solution
- Recommended to you
- Outline