MindMap Gallery Formation and dissociation of complex compounds
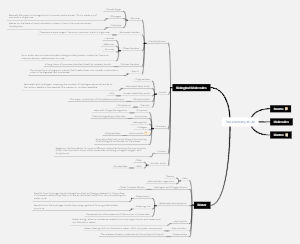
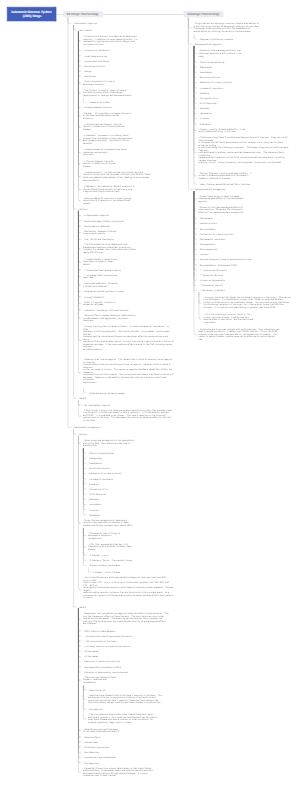
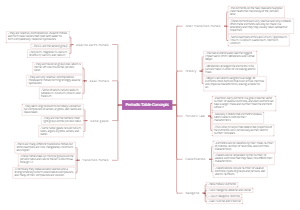
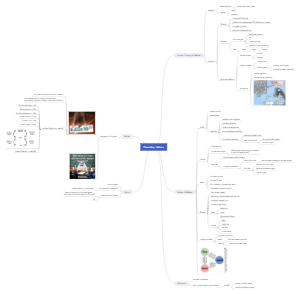
Formation and dissociation of complex compounds
Complex compounds are formed when metal ions bind to ligands, such as water, chloride, or organic molecules, through coordinate covalent bonds, resulting in stable and often colorful species. Dissociation occurs when the coordinate covalent bonds between the metal ion and ligands are broken, often due to changes in conditions such as temperature, pH, or the presence of competing ligands. Analytical techniques such as spectrophotometry, electrophoresis, and NMR spectroscopy are used to analyze the composition, stability, and structure of complex compounds.
Edited at 2024-12-17 07:21:07Formation and dissociation of complex compounds
- Recommended to you
- Outline